Zimbabwe's Initial Encounter with Mpox: A Concern for Public Health
Zimbabwe has stepped into uncharted territory with the recent confirmation of its first two cases of mpox. This revelation, announced by the health ministry, draws attention to the global proliferation of this disease. The ministry's report intriguingly omitted any mention of the specific variant involved, an absence that has stirred both curiosity and concern across the populace. Zimbabwe, having thus far avoided mpox, must now grapple with the complexities of disease management and containment strategies amidst a climate of uncertainty. The lack of detailed information, from the whereabouts of the cases to their medical conditions, has led to an atmosphere of speculation as health officials work diligently to address the repercussions.
The Mystery Variant and its Implications
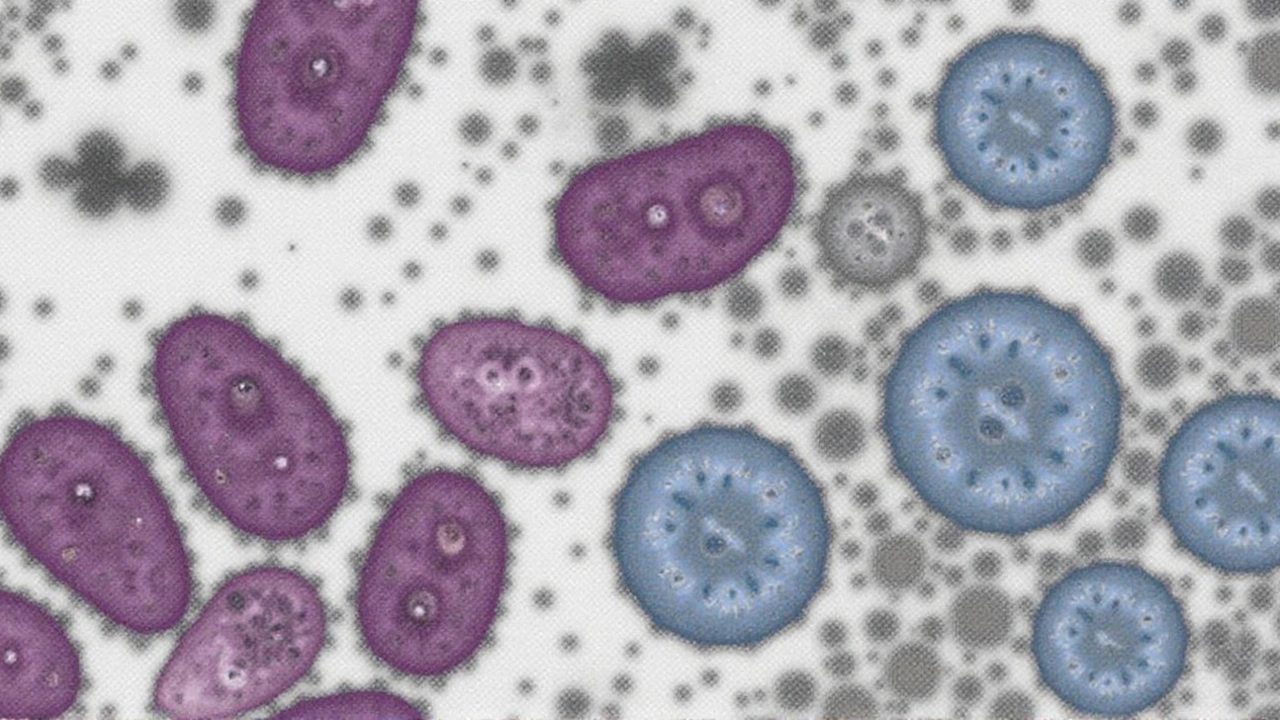
The unspecified nature of the mpox variant found in Zimbabwe's cases adds an air of mystery to the announcement. Mpox, known scientifically as Monkeypox, is a rare viral zoonosis primarily found in Central and West African regions. The disease can transmit from animals to humans, underscoring the importance of identifying the variant's characteristics to inform public health responses and preventive measures. Without this critical knowledge, predicting the outbreak's trajectory becomes challenging, leaving the health ministry to play a precarious balancing act of managing public safety and maintaining calm.
The Response: Managing Public Health Concerns
Zimbabwe's health authorities face an immediate challenge—creating a robust response plan while operating with limited detailed data. Public health measures may include contact tracing, isolation protocols, and public advisories on hygiene practices. Health officials may also ramp up surveillance to monitor for potential spread within communities. Transparent communication remains a critical element of this response strategy, ensuring that the public remains well-informed about developments and understands the importance of adhering to health guidelines.
Understanding Mpox and its Symptoms
Mpox symptoms, which often mirror those of more common infections, can include fever, rash, and swollen lymph nodes. While typically less transmissible than other viral infections, its recent appearance in Zimbabwe raises questions about potential shifts in transmission dynamics or viral evolution. Understanding the disease's signs and symptoms allows healthcare providers to identify potential cases swiftly and administer appropriate care. Moreover, promoting awareness about Mpox among the public can help in early detection and containment efforts.
The Global Context: Mpox in the Modern Era
In recent years, Mpox has gained unprecedented attention, primarily due to its emergence outside traditional geographic confines. This globalization of the viral threat highlights vulnerabilities within global health infrastructures, challenging countries to reassess their readiness for disease outbreaks. Zimbabwe's recent cases serve as a reminder of the interconnected nature of health phenomena, urging international collaboration to mitigate potential crises effectively.
Future Steps for Zimbabwe
The task ahead for Zimbabwe involves navigating an intricate landscape of public health policy, resource allocation, and international cooperation. Securing vaccines and antiviral treatments could be crucial steps in enhancing the country's preparedness for any potential escalation. Furthermore, partnerships with global health organizations could provide expert advice and additional resources necessary to manage this health predicament. Being a part of the broader narrative, Zimbabwe's response to Mpox could serve as a valuable lesson for other nations encountering similar challenges.

Comments (12)
Seeing Zimbabwe stumble into the mpox arena feels like a stark reminder that no nation is insulated from the global virus parade. The lack of transparency mirrors the same bureaucratic opacity we see in many places that pretend to be immune. It's almost philosophical: a disease doesn't respect borders, yet we keep building imaginary walls. The real tragedy is that the world watches in silence while officials scramble for vague answers. If we don't demand accountability now, we'll be shouting louder when the next outbreak hits our doorstep. The unnamed variant is a red flag, a silent alarm that should shake even the most complacent governments. In this era, the only sensible stance is to treat every outbreak as a personal affront to global health safety.
😭 this is heartbreaking! The uncertainty and lack of info is just *so* painful for everyone watching. 🙏 stay safe, Zimbabwe, and please keep us updated! 😢
Alright, let’s break this down for the folks who want the full picture. First, mpox, also known as monkeypox, is a zoonotic virus that primarily spreads from animals to humans, but human‑to‑human transmission is definitely possible, especially with close contact. The two confirmed cases in Zimbabwe are just the tip of the iceberg – without thorough contact tracing, we can’t know how many others might have been exposed. Second, the variant hasn’t been named, which means we lack crucial data on its transmissibility, virulence, and potential resistance to existing antivirals. Third, the typical incubation period for mpox is 7‑14 days, so anyone who was in contact with the patients could develop symptoms any time soon. Fourth, common symptoms include fever, rash, and swollen lymph nodes – these overlap with many other illnesses, making clinical diagnosis tricky without lab confirmation.
Fifth, the key public health tools are isolation of confirmed cases, meticulous contact tracing, and vaccination where possible. The Jynneos vaccine, which is approved for mpox, can help curb spread if administered quickly to close contacts. Sixth, countries with robust surveillance systems have reported declines after aggressive vaccination campaigns, so Zimbabwe would benefit from securing doses promptly.
Seventh, global collaboration is essential. The WHO, CDC, and local ministries need to share genomic data to pinpoint the variant and assess if it differs from the West African or Congo‑ Basin strains. Eighth, community education is vital – people need to know how the virus spreads and the importance of reporting symptoms early.
Ninth, despite the fear, mpox isn’t as contagious as COVID‑19, but complacency is dangerous. Tenth, the economic impact of an outbreak can be significant, affecting tourism and trade, so swift action can mitigate longer‑term losses.
Eleventh, health workers should wear appropriate PPE to avoid nosocomial transmission. Twelfth, mental health support for patients and contacts is often overlooked but equally important.
Thirteenth, the lack of detailed reporting from the Ministry may be due to stigma or resource constraints, but transparency builds public trust.
Fourteenth, neighboring countries should be on alert, as cross‑border travel can facilitate spread.
Finally, staying informed, following official guidance, and supporting vaccination efforts are the best ways we can help contain this outbreak.
Thanks for the thorough rundown, Amy. It’s reassuring to see so many practical steps laid out. I’m hopeful that if the health ministry leans into transparent communication, the public will stay calm and cooperative. Remember, early detection and community support can make a huge difference.
Interesting. Zimbabwe should focus on contact tracing and quick vaccination. Minimal jargon is best.
Agreed. A balanced approach that respects cultural nuances while enforcing strict health protocols will be most effective. Collaborating with WHO experts can provide the needed technical support, and securing vaccine supplies should be a priority. Let’s hope the ministry acts decisively.
Isn't it wild how a tiny virus can expose how connected our world truly is? Maybe it's time we all think a bit deeper about our shared responsibility.
Honestly, the whole thing reeks of mismanagement. The ministry's vague statements are exactly what you expect when they’re clueless. They should've been prepared-no excuse for this level of incompetence.
🤔 I'm curious about the vaccine rollout plans. Will they prioritize healthcare workers first? Also, any chance we see regional cooperation with nearby countries? 🌍
Looks like another example of the elite hiding the truth. Who knows what they're covering up? The virus could be engineered to keep us scared while they profit.
From a philosophical standpoint, disease outbreaks force societies to confront their fragility and the ethical obligations we owe each other. While the immediate response is crucial, the long‑term lesson lies in building resilient health infrastructures that honor the dignity of every individual.
Got it.